Why AI is the next frontier of medicine
During Google’s (GOOG, GOOGL) massive developers conference in early May, CEO Sundar Pichai took the stage to detail how its latest research in artificial intelligence could one day help doctors detect heart disease. What’s more, the AI system, which based its findings on scans of patients’ retinas — a method known to provide clues to a person’s heart health — was nearly as accurate as traditional blood tests.
It was an impressive reveal that drew an enormous round of applause from the audience at Shoreline Amphitheatre in Mountain View, Calif. But it’s only a small piece of a larger body of research the technology and medical communities are quickly piecing together in their quest to create AI systems that could eventually save countless lives — including your own.
An AI heart test
“To me, it seems obvious that this is the next natural step in which medicine should head,” said Dr. Sanjay Desai, director of the Osler Medical Training Program at Johns Hopkins School of Medicine.
Google’s eye test used a form of AI called machine learning, which attempts to teach a computer system how to make decisions by feeding tons of data into an algorithm.
To do that Google fed its algorithm images of both normal retinas and those of people who show signs of heart disease, an approach called computer vision. After training the algorithm, it was able to look at individual images of retinas and determine whether they belonged to healthy patients or those who may have heart disease.
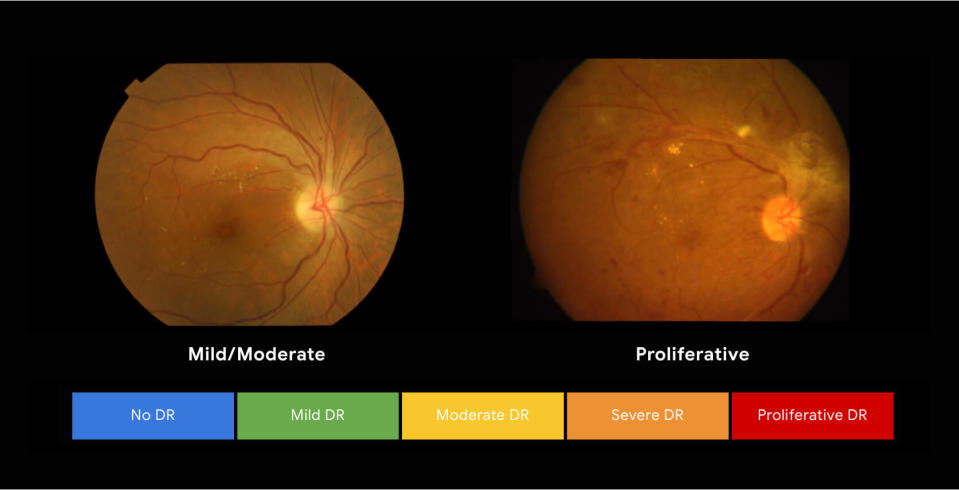
Google previously used machine learning to prove it can identify individuals at risk of diabetic retinopathy, a disease that can cause irreversible blindness if left untreated. After training its algorithm, the search giant said its machine learning system was as accurate as trained ophthalmologists in identifying signs of the disease. Another machine learning algorithm identified tumors in breast tissue.
Moving beyond photos
Computer vision technology can be incredibly useful in imaging, but it’s far from the only way researchers are using AI in the medical field.
At the Stanford University School of Medicine, Dr. Josh Knowles is using patients’ electronic health records (EHRs) to identify previously undiagnosed individuals with familial hypercholesterolemia (FH), a genetic heart condition that affects 1 in 250 people and results in a high chance of early onset heart disease and heart attacks if left untreated. According to Knowles, about 1 million people in the U.S. have FH, but just 10% have been diagnosed.
“The idea behind the project is that we know there’s a lot of FH patients out there … that have not been diagnosed. But if we found them, we could treat them,” Knowles explained.
FH is an autosomal dominant disease, which means if you have it, you’ve inherited it from your parents and can pass it on to your children. So identifying one patient could allow doctors to help multiple family members.
To determine if someone had FH, Knowles said Stanford researchers fed entire medical records of individuals with and without FH, including text notes, prescriptions, diagnostic tests and medications into a classification algorithm that used the data to identify a pattern consistent with FH patients.
“It’s like analogous to your email system learning what spam is,” Knowles explained. “You just show it a bunch of examples of spam, and it knows what spam is.”
Knowles said researchers then pulled the charts of those individuals the algorithm identified as likely having FH and found the system performed about as well as a human in diagnosing patients.
“You could imagine this happening for … many potentially important conditions, not just FH,” Knowles said.
Predicting patient reactions
At the Cleveland Clinic researchers and doctors are using machine learning to predict the wellbeing of certain patients.
“We’re doing things to help us identify high-risk patients,” explained Cleveland Clinic’s Executive director of enterprise information management and analytics Chris Donovan. “So what patients are at risk of being admitted, what patients are at risk of deterioration in their care, or in their clinical condition and how do we intervene on those patients proactively.”
The hospital is also looking into using machine learning to determine if certain patients are good candidates for a specific type of surgery.
“Through 20 years of research and multiple randomized control trials where you isolate all of the variables except for one and follow that variable out over to time to see does this have an impact or does it not, we still know that we’re not very good at choosing who’s going to have a good outcome, or discerning is a better word, who’s going to have a good outcome and who is not,” said the Cleveland Clinic’s Dr. Timothy Crone.
Guiding treatments
At Johns Hopkins, Desai says, work is being done with The Human Diagnosis Project to determine how physicians make decisions and treat patients. The project, according to its website is, “a worldwide effort, created with and led by the global medical community, to build an open intelligence system that maps the steps to help any patient.”
“What we’re working on now is trying to understand how physicians make decisions in today’s environment with all of the data they have,” Desai explained. “We try to sit with people who are considered master clinicians and actually talk through and try to learn how they solve cases.”
Ultimately, such a project could give doctors around the world a better understanding of how to successfully treat patients with any kind of ailment.
An artificial doctor?
Despite what research has shown, it’s important to note that doctors aren’t actively using AI or machine learning to diagnose patients in the real world. Instead, they’re testing to see how well the technology can be used in the future to inform doctors’ decisions. In other words, don’t go into your local doctor’s office asking for a machine to diagnose your runny nose.
“I think there is a ton of potential; I think there’s still a long way to go,” Donovan said. “I think there is a lot of hype. You know the idea that you can use AI to cure cancer today is really overblown. But to improve how we’re doing our work is huge.”
When the technology is fully fleshed out, though, will we say goodbye to our flesh-and-blood physicians? According to Knowles, that scenario is highly unlikely.
On a practical level, these algorithms are designed with a single goal in mind: identifying a condition or treatment method for one very specific issue. They don’t have the level of institutional knowledge a real-life doctor has amassed through years of study and training.
And on a more human level, there’s the ability for doctors to discuss problems and empathize with their patients.
“There is much more to medicine than diagnosing radiological images. It’s really the doctor patient relationship, or the provider patient relationship,” he said. “It’s more about, you know, values and understanding what people want and need, and emotional connection and things, and I don’t think that computers are going to take the spot of us.”
AI will certainly become a part of our lives in the future, similar to how computers are now a major part of our lives — but don’t expect it to replace your family physician anytime soon.
Correction: A quotation from Dr. Timothy Crone was incorrectly attributed to Chris Donovan. The error has been corrected.
More from Dan:
Apple CEO Tim Cook brings up data privacy in Duke graduation speech
Warren Buffett: ‘Cyber is uncharted territory and it’s going to get worse, not better’
This is the closest you can get to a ‘Star Wars’-style lightsaber battle
Email Daniel Howley at [email protected]; follow him on Twitter at @DanielHowley. Follow Yahoo Finance on Facebook, Twitter, Instagram, and LinkedIn
