Coronavirus or the flu? 'Impossible to distinguish' between the two without testing, doctor says
The changing of the seasons isn’t good news for public health purposes.
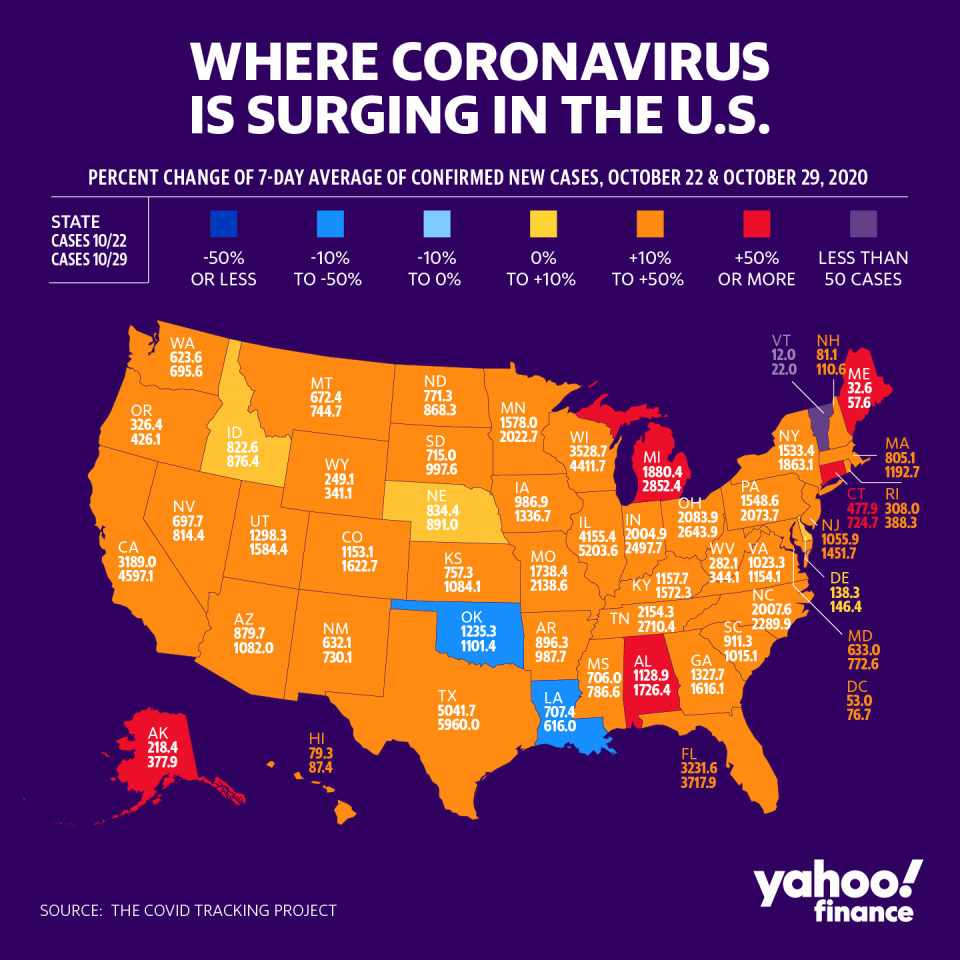
As the U.S. continues grappling with significant spikes in coronavirus cases, the country is now also facing flu season (from roughly November through February). To make matters worse, it’s next to impossible to distinguish the two illnesses, according to one expert.
“We’re definitely concerned about our testing capacity,” Dr. Taison Bell, an assistant professor of medicine in the infectious disease and pulmonary divisions at the University of Virginia, said on Yahoo Finance. “It is very hard to distinguish — actually impossible to distinguish — patients who have the flu versus the coronavirus versus the other respiratory illnesses that we have in the winter that all surge. So our testing capacity needs to be way greater than where it is right now.”
‘It’s here and it’s surging’
The symptoms for coronavirus and the flu virus are largely similar. Both involve a fever, body aches, and chills, and both can cause pneumonia, a serious lung infection. Both are infectious and potentially lethal, though COVID-19 — the disease caused by coronavirus — seems to be much more infectious and deadly.
Some of the key differences include how many COVID-positive patients lose their sense of taste and smell and that many are often asymptomatic but still pass the virus on to others. There is no known cure for the coronavirus, although numerous pharmaceutical companies are in the process of developing a vaccine. The flu, on the other hand, has a vaccine that is offered each year to lower your risk of contracting it.
“We’ve seen how cases can overrun hospital systems and have capacity reached in ICUs or exceeded,” Bell said. “In some cases, patients being transferred out of the state to get care because there aren’t enough resources to take care of these patients. And along with that goes our PPE supply, the health of our staff, and our employees who work in these hospitals. Because the cold and flu season affects us too.”
Hospital staff would be previously able to come to the hospital if they had a cough or “the sniffles,” as long as they didn’t have a fever. But now, everything is considered a risk until proven otherwise.

As a result, Bell said, “I do think there’s going to be a lot of staff outages as well as capacity reach and maybe strains on testing in some areas of the country.”
The rise in coronavirus cases at the same time as flu season is a nightmare for any health professional.
“We were afraid that we would have a lot of cases going into the cold and flu season,” Bell said. “We’re having more cases growing faster than testing. Our percent positivity in some states is frighteningly high. Now we want it below at least 10% but ideally below 5%.”
In some states and regions, the positivity rate is even higher. For example, Wyoming has seen a 23.6% increase in cases week over week, the largest among any state. Not far behind are Alaska at 20.5%, Montana at 20.3 %, South Dakota at 19.4%, and North Dakota at 17.3.
“Regardless of what you want to call it, it’s here and it’s surging,” Bell said.
What wave are we in?
So far, the U.S. has administered over 142 million tests for COVID-19 since the pandemic began earlier this year. On Oct. 29, the most recent day with data available, over 240,000 tests were conducted, yielding over 88,000 positive results.
But the confirmed cases trend is continuing to go upward, with as many positive cases as there were back earlier on in the pandemic in some states.
“I’m not really interested in calling this a first wave or a second wave,” Bell said. “I personally think we did not actually control the first wave. But regardless of what you want to call it, our cases are frighteningly high. And this is exactly what public health officials and infectious disease doctors were afraid of when we saw the virus persisting, despite the warmer summer months.”

Some officials, including President Trump, have attributed the rising cases to the increased availability of testing. But Bell brushed off that notion.
“Cases are now up 50%, compared to this time or the earlier part of this month,” he said. “Our testing has only gone up by 13%. So those who say that the increased cases are explained by testing, that’s not true at all.”
To gain control of the spread of the virus, Bell recommended that certain measures be put in place.
“I think we can have some of these activities that we’re doing, with some restrictions in place where we see cases surging,” he said. “But it has to be paired with smart public health practices, wearing a mask at all times, especially indoors, spatial distancing six feet at least, and frequent hand hygiene, and trying to avoid enclosed spaces.”
He added that we “absolutely have to do these measures now, or we’re going to have bad news the next couple of weeks.”

The U.S. is on track to surpass 500,000 deaths by February 2021. And according to Dr. Anthony Fauci, the director of the National Institute of Allergy and Infectious Diseases (NIAID), there likely won’t be a return to normalcy until early 2022.
“I don’t have a specific projection, but we’ve seen this play out before,” Bell said. “When we have cases going up and we’re not implementing these public health measures and lockdowns that we need to, cases are just going to keep rising, and eventually hospitalizations will increase. We’re already seeing that in several states and across the country.”
He continued: “Then eventually, deaths will start to rise, too. And that’s when people will start self-imposing restrictions and not going out and not participating in the economy. This argument that we either have to choose public health or the economy is a false argument because I really think they are partners together.”
Adriana Belmonte is a reporter and editor covering politics and health care policy for Yahoo Finance. You can follow her on Twitter @adrianambells.
READ MORE:
Americans increasingly turn to free health care clinics amid loss of employer-sponsored plans
How the coronavirus impacts whether or not patients seek care for other health problems
Doctor: US clearly in a 'third wave' of coronavirus infections as COVID-19 fatigue sets in
Read the latest financial and business news from Yahoo Finance
Follow Yahoo Finance on Twitter, Facebook, Instagram, Flipboard, LinkedIn, YouTube, and reddit.
