'It didn't have to be this way': Nurses describe brutal toll of treating coronavirus patients in America
Members of a prominent nurses union shared ongoing struggles involving coronavirus patients recently at a virtual roundtable with former Second Lady Jill Biden.
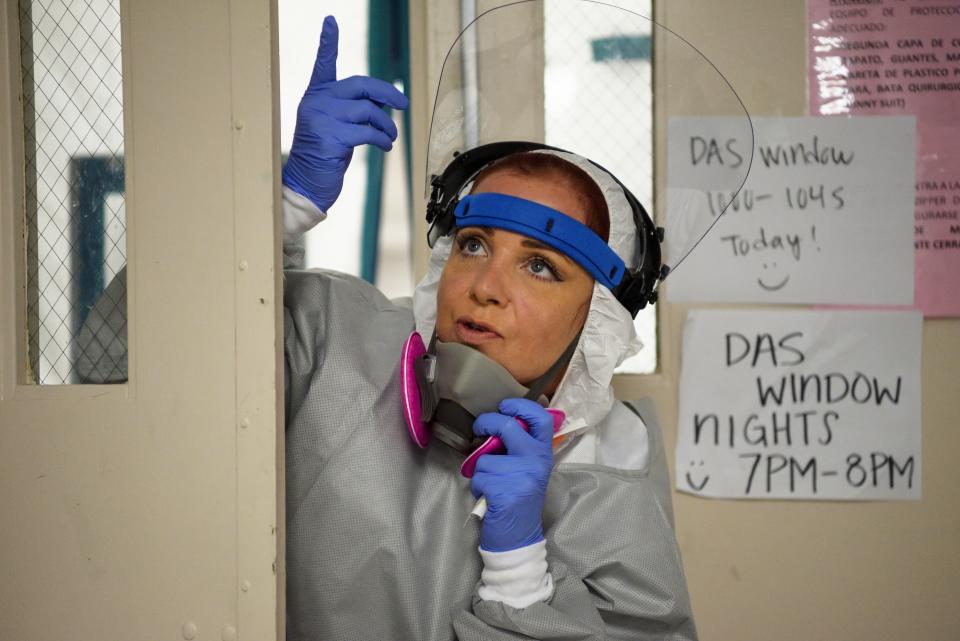
“We have a supply person who comes to our unit and hands out the N95s for that shift,” Christine Valenzuela, a registered nurse (RN) based in Arizona, said on the September 12 video chat organized by National Nurses United (NNU). “One time in the ICU, our supply person was over 40 minutes late getting to my unit. My patient was crashing and about to code. And I didn’t have a respirator to go into that room.”
At that point, Valenzuela added, “we had to quickly scramble and were able to find another nurse who had an N95 so that they could go save the patient. I’ve been a nurse for 13 years, and I have never experienced this before where everyone’s safety is at risk because we can’t easily retrieve a respirator when we just simply need one.”

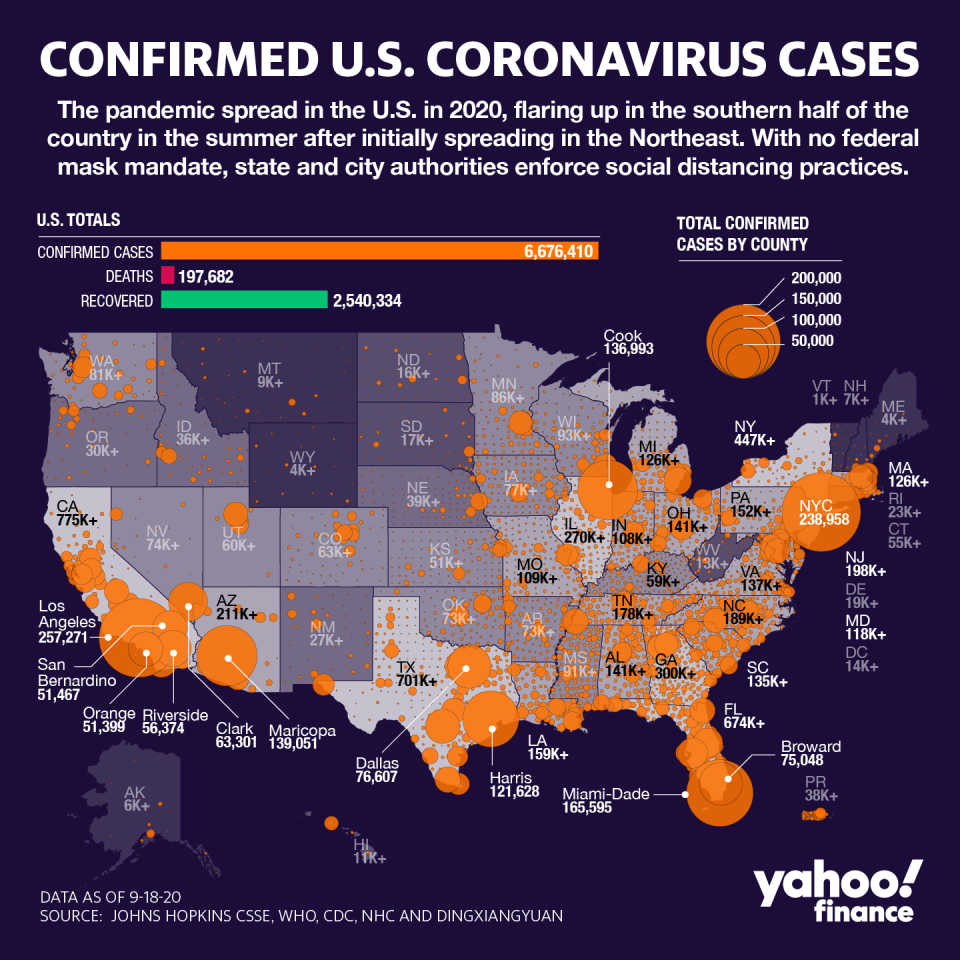
Although the U.S. is now more than six months into the pandemic, there are still shortages of personal protective equipment (PPE), particularly N95 respirators, which are considered the safest masks for health care providers to use while treating patients.
Public officials have stated that at least 3.5 billion masks are needed this year, and the U.S. is still lacking.
“We are eight months into this pandemic, and you still don't have the protective equipment you need,” Biden said to the roundtable of nurses. “We're still hearing stories about nurses not having the supplies they need, or reusing N95 masks. It's a disgrace to the people working on the front lines and all Americans. It didn't have to be this way.”
A July 2020 survey from NNU over more than 21,200 nurses found that 87% of nurses reported having to reuse at least one piece of PPE while working at a hospital. Only 24% of respondents thought their employer is providing a safe workplace.

‘A single N95 respirator’ to reuse
When the Centers for Disease Control & Prevention (CDC) changed its guidance on protective gear in March, some hospitals were immediately affected.
According to Vanessa Evans, a nurse who works in the Intensive Care Unit (ICU) of MountainView Hospital in Las Vegas, all of the hospital’s PPE was locked up in storage, which she described as “unnerving” for her and her colleagues.
Evans admitted one of the first suspected coronavirus patients to the ICU, but “due to the confusion, lack of protocols, and lack of testing in place to address this pandemic, I was told by our administration to not implement precautionary measures for my patient until they tested positive for COVID-19,” she said. “Instead, I was to test them for every other type of virus that we currently had a test for. And if they tested positive for any of those, we were not to test them for COVID-19.”
And because there is no clear federal plan, hospitals have had to grapple with shortages of supplies and tests on their own. At MountainView, according to Evans, hospital administration approved any testing.
“The physicians were not allowed to control those decisions,” she said. “Furthermore, if we wanted protective equipment, we would have to go through a chain of command and get approval. Our charge nurse had to go to three different doctors in the hospital to get me — one nurse — a single N95 respirator, which I was to reuse as well as eye protection in the form of goggles.”
She added that there was “also a lack of clarity on the availability and usage of our single use medical gowns. And we were ultimately instructed to reuse them unless visibly soiled, putting used gowns back on for the same patient, and attempting to move from least contaminated patients to most contaminated patients.”
MountainView Hospital did not respond to request for comment.
‘I was very sick’
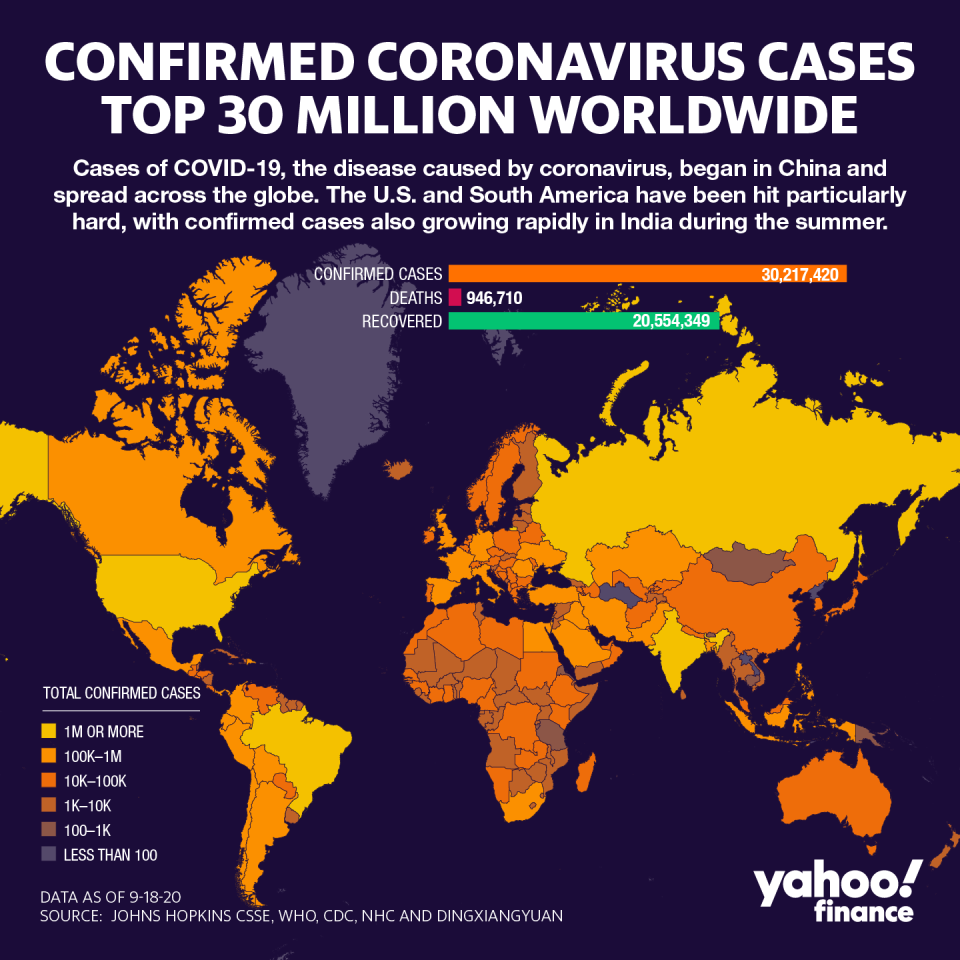
Worldwide, over 90,000 health care workers have tested positive for the virus and more than 7,000 have died from COVID-19, the disease caused by coronavirus.
In some cases, poor protective guidelines have led these numbers.
This happened to Dominique Hamilton, an RN based out of Arizona who works in a unit that specializes in orthopedics and neurology. She became ill at the beginning of March and was denied a COVID test several times until finally getting one and testing positive.
“I was very sick,” Hamilton said. “I was in bed for a month. I had to take time to even begin to walk again in the second month. It was extremely difficult dealing with the shortness of breath and fatigue. I visited the emergency room twice, because as a health care professional and hearing stories of how quickly this can get bad, I knew that the second and third weeks were pretty crucial to make sure that my health was being monitored.”
And though she’s recovered since then, it was a slow process. Hamilton had to see a pulmonologist and wasn’t able to go back to work until three months later.
“This has been a life-changing experience for me — a very emotional experience,” she said. “I’m 29 years old. And the only health history I have is mild asthma. I live in a full house. It was very anxiety-inducing to be separated in a room the majority of that time. I was terrified that I would infect anyone who came around me.”
That’s not her only fear, either.
“The fear of being unwell chronically stays with me,” she said. “On top of that, the fear I might faint at work. I fainted before in the grocery store. It’s difficult to talk about these fears, quite honestly, because nurses are expected to show nothing but strength and resilience.”
She added that the “martyrdom that we take on as nurses, as women, as women of color, we must end that. When we’re taking care of patients without protections, we aren’t strong. We’re vulnerable. We feel scared for our patients, ourselves, our families, our communities. We resolved to tell the truth about the realities of this pandemic.”
Biden, wife of Democratic presidential candidate Joe Biden, told Hamilton at one point that “our nation owes you an enormous debt of gratitude. It really is unconscionable in our country that you don't have what you need to do your job.”
Adriana is a reporter and editor covering politics and health care policy for Yahoo Finance. Follow her on Twitter @adrianambells.
READ MORE:
Nurses lobby for better conditions after U.S. coronavirus havoc
How coronavirus ravaged a nursing home industry that was already 'in crisis'
Read the latest financial and business news from Yahoo Finance
Follow Yahoo Finance on Twitter, Facebook, Instagram, Flipboard, SmartNews, LinkedIn, YouTube, and reddit.
